Informed consent (Medical law)
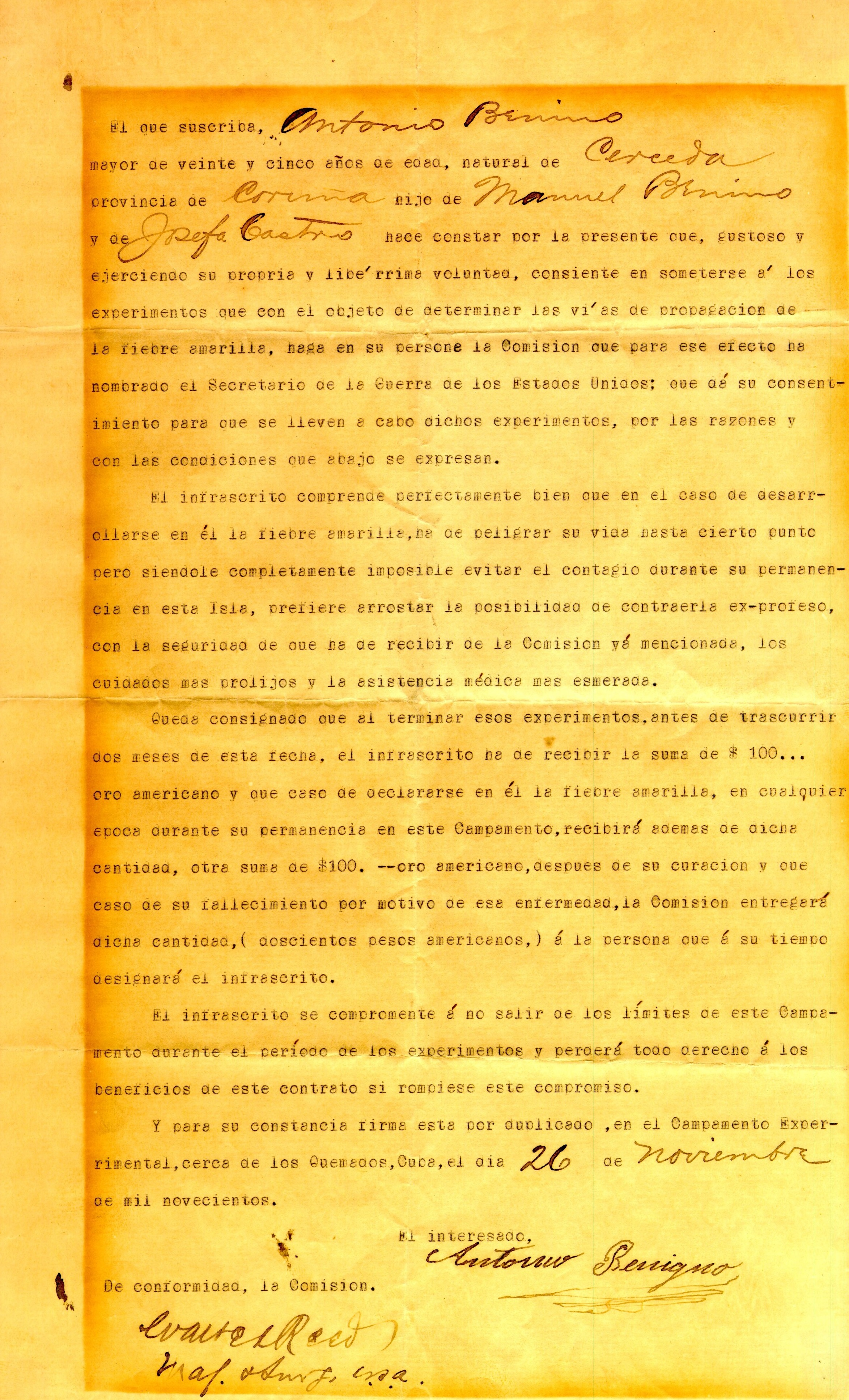
Enlarge text Shrink textInformed consent is a principle in medical ethics, medical law, media studies, and other fields, that a person must have sufficient information and understanding before making decisions about accepting risk, such as their medical care. Pertinent information may include risks and benefits of treatments, alternative treatments, the patient's role in treatment, and their right to refuse treatment. In most systems, healthcare providers have a legal and ethical responsibility to ensure that a patient's consent is informed. This principle applies more broadly than healthcare intervention, for example to conduct research, to disclose a person's medical information, or to participate in high risk sporting and recreational activities. Within the US, definitions of informed consent vary, and the standard required is generally determined by the state. These standards in medical contexts are formalized in the requirement for decision-making capacity and professional determinations in these contexts have legal authority. This requirement can be summarized in brief to presently include the following conditions, all of which must be met in order for one to qualify as possessing decision-making capacity: Choice, the ability to provide or evidence a decision. Understanding, the capacity to apprehend the relevant facts pertaining to the decision at issue. Appreciation, the ability of the patient to give informed consent with concern for, and belief in, the impact the relevant facts will have upon oneself. Reasoning, the mental acuity to make the relevant inferences from, and mental manipulations of, the information appreciated and understood to apply to the decision at hand. Impairments to reasoning and judgment that may preclude informed consent include intellectual or emotional immaturity, high levels of stress such as post-traumatic stress disorder or a severe intellectual disability, severe mental disorder, intoxication, severe sleep deprivation, dementia, or coma. Obtaining informed consent is not always required. If an individual is considered unable to give informed consent, another person is generally authorized to give consent on the individual's behalf—for example, the parents or legal guardians of a child (though in this circumstance the child may be required to provide informed assent) and conservators for the mentally disordered. Alternatively, the doctrine of implied consent permits treatment in limited cases, for example when an unconscious person will die without immediate intervention. Cases in which an individual is provided insufficient information to form a reasoned decision raise serious ethical issues. When these issues occur, or are anticipated to occur, in a clinical trial, they are subject to review by an ethics committee or institutional review board. Informed consent is codified in both national and international law. 'Free consent' is a cognate term in the International Covenant on Civil and Political Rights, adopted in 1966 by the United Nations, and intended to be in force by 23 March 1976. Article 7 of the covenant prohibits experiments conducted without the "free consent to medical or scientific experimentation" of the subject. As of September 2019, the covenant has 173 parties and six more signatories without ratification.
Read more on Wikipedia >
 Topic
Topic